38 Weeks Pregnant
At 38 weeks gestation, you’re closing in on the finish line, with just a couple more weeks to go until your due date. As your body experiences the final stages of pregnancy around your 38th week, you might notice a variety of symptoms signalling that labour could be right around the corner. Let’s explore what you might experience at 38 weeks pregnant, including the signs of labour and some things to help you prepare during this stage.
Highlights at 38 Weeks Pregnant
Here are a few highlights from 38 weeks of pregnancy:
Your baby is taking up a lot of space in the amniotic sac, and there isn’t much room for rolling or turning.
At 38 weeks, your baby may be in a head-down position in preparation for the trip through the birth canal.
Get as prepared as you can for giving birth by selecting your labour partner, being aware of the signs of labour, and knowing when to head to the hospital at around 38 weeks.
Still searching for the perfect name for your little one? If so, try our Baby Name Generator, with so many great options to choose from:
RELATED PREGNANCY TOOL
Baby Name Generator
Filter by gender:
Filter by theme:
38 Weeks Pregnant: Your Baby’s Development
At 38 weeks pregnant, your little one is close to making their debut yet they’re still developing each day. Take a look at what’s happening right now:
In these final few weeks, your baby’s brain is still growing. In fact, your baby’s brain can grow as much as one-third in size between 35 and 39 weeks pregnant. You knew your little one was a genius!
Your baby’s liver is nearly fully developed at this time, too.
After your baby is born, their first few bowel movements will be a substance called meconium. This greenish-black, sticky form of poop starts to build up in the intestines while your baby is still in the uterus, formed from waste materials such as dead skin cells and lanugo, the fine body hair your little one is starting to shed.
Even though your estimated due date is still a couple of weeks away when you’re at 38 weeks, you may start to notice some signs of labour approaching, and your baby could arrive any day now. Only about five percent of pregnancies deliver exactly on the due date.
Twins and other multiples are more likely to be born preterm than a single baby, so keep an eye out for signs and symptoms of labour if you’re 38 weeks pregnant with twins.
38 Weeks Pregnant in Months
How many months is 38 weeks pregnant? Since pregnancy doesn’t divide neatly into months, you may find the answers vary. At 38 weeks pregnant, you’re generally considered 9 or 10 months pregnant.
Baby’s Size at 38 Weeks Pregnant
At 38 weeks pregnant, the average baby is about the size of a bunch of rhubarb, and their weight could be approaching 7 pounds—in kg that’s about 3.2 kilograms.
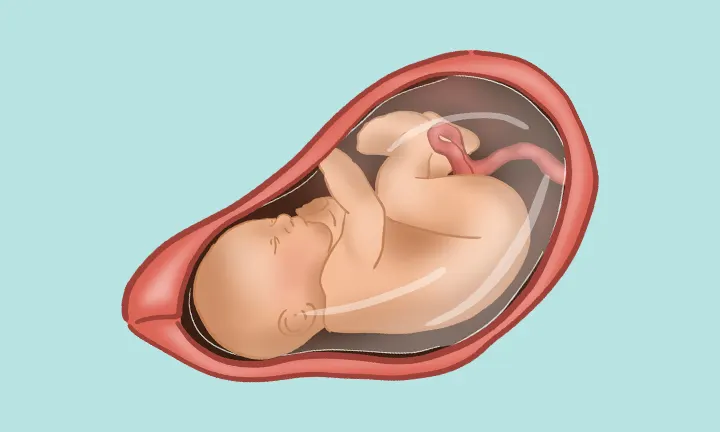
Your Baby: What Does 38 Weeks Pregnant Look Like?
Wondering how your little one might be positioned at 38 weeks? At this stage, your baby may have dropped lower into the pelvis. Here’s a general idea of what your little one might look like:
Your Body at 38 Weeks Pregnant
At 38 weeks pregnant, you may still be gaining weight, believe it or not. If you had a normal body mass index (BMI) before you were pregnant, you’ll likely put on between half a pound and one pound per week during the third trimester. To find out more about your estimated weight gain in these final few weeks, take a look at our pregnancy weight gain calculator.
Your ever-growing belly might be getting in the way of a good night’s sleep (and normal movement) these days, but the end is in sight now!
Some find that getting regular exercise is more difficult at this point. If this is the case for you, you might want to focus on breathing exercises to help get you ready for labour. Not only do these exercises help you relax and de-stress, but they also come in handy to help manage the pain and discomfort of labour.
38 Weeks Pregnant: Your Symptoms
Here are some symptoms you might be experiencing at 38 weeks pregnant:
Frequent urination. As your baby and uterus grow, they’re putting more pressure on your bladder, so you may experience frequent urination at 38 weeks pregnant. Even though those extra bathroom visits are a hassle, keep drinking plenty of water to stay well hydrated.
Pelvic pressure. You and your baby are getting ready for labour in many different ways, and you may feel this in the pelvic area, too. When your baby drops lower into your pelvis, you may feel increased pressure on your pelvis, bladder, and hips. Because your body is producing a hormone called relaxin, which softens the ligaments, muscles, and joints in preparation for childbirth, you might also experience some pelvic or back pain, especially as you get closer to your due date. Try to stay off your feet as much as possible, move slowly and carefully, and soak in a warm bath if you’re feeling uncomfortable.
Swollen ankles and feet. Your body will produce and retain more fluid than usual, and as a result, you may notice swelling (known as edema) in your hands and legs. To combat this, try to rest with your feet up, drink more water to help flush out excess fluid, and wear loose clothes and shoes so you feel a little more comfortable. Some moms-to-be find that wearing support hose or stockings can also help reduce swelling and discomfort. If you notice any sudden swelling in your face or hands, or you’re experiencing severe headaches at 38 weeks pregnant or at any point in your pregnancy, contact your healthcare provider, as this could be a sign of a blood pressure condition called preeclampsia.
Nausea. Some symptoms such as slight nausea and sickness can crop up again at 38 weeks pregnant or in the following weeks, and it can sometimes be a sign that labour is starting. If you’re feeling sick at 38 weeks pregnant, try to eat several smaller meals throughout the day, and stick to bland foods like bananas, rice, or toast.
Contractions. At 38 weeks pregnant, you may have already felt symptoms of Braxton Hicks contractions. These practice contractions usually occur irregularly and will often stop when you move or change positions. On the other hand, true labour contractions will come at regular intervals, getting closer together over time. They’ll increase in strength and intensity, often starting from the back and moving to the front of your abdomen. Timing your contractions will give you more information about whether you’re experiencing the real deal or just more Braxton Hicks. If you experience intense stomach cramps at 38 weeks pregnant or at any point in your pregnancy, or you’re unsure whether you’re experiencing Braxton Hicks or true labour contractions, contact your healthcare provider for more advice.
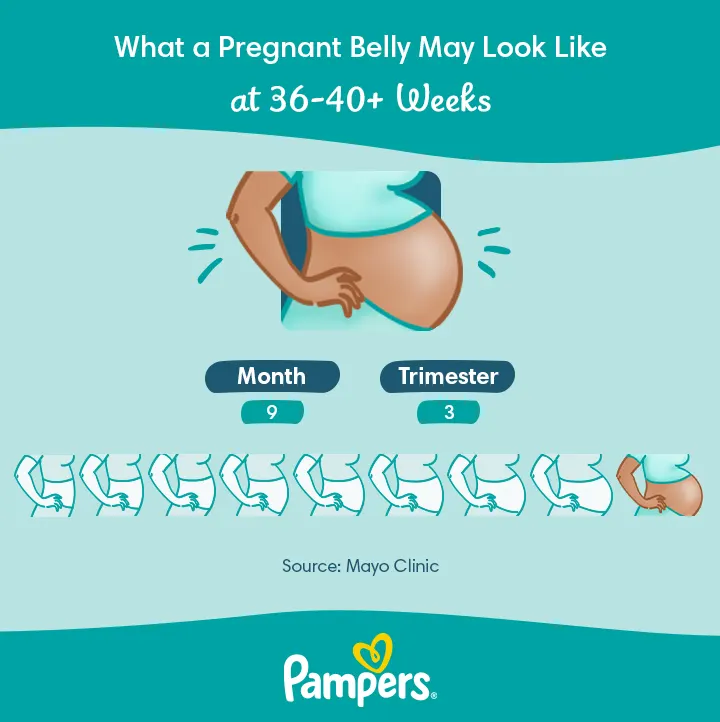
How Big Is a Pregnant Belly at 38 Weeks?
You’re nearly at the end of your pregnancy, and your uterus will finish expanding this month. At the start of your pregnancy, your uterus could have weighed around 2 ounces, and now, it may weigh about 2½ pounds.
What Does 38 Weeks Pregnant Look Like?
For a general idea of what your belly might look like at 38 weeks pregnant, take a look at the image below.
38 Weeks Pregnant: Things to Consider
As your due date approaches, here are a few things to consider:
Have you considered your options for pain relief during your labour? If you haven’t, reach out to your healthcare provider. Pain relief drugs are typically either analgesic, which usually lessens but doesn’t stop the pain, or anesthetic, which stops you from feeling any pain. One well-known pain relief option is the epidural, but your healthcare provider is the best person to ask about what could be right for you. If you’ve taken a childbirth class, you may have also learned about comfort techniques like the Lamaze, Bradley, and Read methods. Consider all your options, and talk over your preferences with your provider.
You may want to choose a birth partner who will be with you throughout your labour and delivery. This person can be your partner, a family member, a friend, or even a trained professional, like a doula. Your birth partner can support you emotionally and provide encouragement. They can also give practical assistance like timing contractions or offering a soothing massage, for example. Medical studies show that pregnant people who have continuous labour support often have shorter labours and require less pain medication. But, no matter what, you won’t be going it alone when the big day comes. Your hospital or birthing centre staff will be with you every step of the way.
Find out your hospital or birth centre’s policies on eating and drinking during labour. If you know you’ll be having a caesarean section, you’ll need to restrict your food intake before surgery. Your healthcare provider will be able to give you more information on how long you’ll need to fast for. For a vaginal delivery, it may be possible to have small amounts of clear liquids during labour (think ice chips!), but you may not be allowed to eat solid foods. Check with your provider or hospital staff in advance to be sure.
If you’re considering breastfeeding your baby, you might like to research lactation consultants in your area. A lactation consultant can help you get started and navigate any possible challenges associated with breastfeeding your baby, such as getting the proper latch or dealing with sore nipples. Your hospital or birthing centre may have a lactation consultant on staff, and your healthcare provider may also be able to recommend someone.
Consider taking some time this week to read up on the postpartum period. Knowing ahead of time what might occur could help you feel more prepared for those first weeks and months. We’ve collected some articles here that you may find interesting:
Tip for Partners
|
38 Weeks Pregnant: Questions for Your Healthcare Provider
It won’t be long until your little one is in the world, so take this time to ask your healthcare provider any questions you might have. These might include:
Is there anything I can do from here on out to prepare for labour?
What are some symptoms not to ignore at 38 weeks pregnant?
Is it safe to have sex during the final weeks of my pregnancy?
Under what conditions might it be necessary to induce labour, and how common is induction at 38 weeks pregnant?
What is recommended if my baby is in a breech position?
If I think I’m in labour, who should I call? Should I call straight away or wait for something specific?
I’ve had breast implants or other breast surgery. Can I still breastfeed my baby?
How soon can I start breastfeeding after giving birth?
FAQs at a Glance
As you approach the final stretch of your pregnancy, you might want to focus on self-care and preparation. Ensure you attend any upcoming prenatal appointments, check that all essential items for the baby are ready, and finalize any outstanding tasks to alleviate stress as your due date approaches.
38 Weeks Pregnant: Your Checklist
You can use our checklist for some handy to-dos during this period of your pregnancy:
You may have already started packing your hospital bag, but you might not have been able to pack things you’re still using, like your phone charger and toothbrush. Make a list of these items or go through our downloadable hospital bag checklist, so you or your partner can throw the last few items in the bag before you go to the hospital.
If you haven’t done so already, have your baby’s car seat installed so it’s ready to bring your baby home safe and sound.
As your due date nears, you may want to check out our free online childbirth education classes—there are nine videos you can watch anytime.
Take some time to pamper and care for yourself—you may not have this kind of “spare time” for a while once your baby is born. For example, you might want to do things like getting a haircut or going for a pampering pedicure.
How We Wrote This Article The information in this article is based on the expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
Join a World of Support